 This is the ninth post in our Winter 2013 blog series Understanding Depression in Kids and Teens…A Primer for Pastors, Church Staff and Christian Parents. Today, we’ll look at the data on the non-pharmacologic treatment with the best supporting evidence in the treatment of children and teens with depression…Cognitive-Behavioral Therapy.
This is the ninth post in our Winter 2013 blog series Understanding Depression in Kids and Teens…A Primer for Pastors, Church Staff and Christian Parents. Today, we’ll look at the data on the non-pharmacologic treatment with the best supporting evidence in the treatment of children and teens with depression…Cognitive-Behavioral Therapy.
Do not conform to the pattern of this world, but be transformed by the renewing of your mind. Then you will be able to test and approve what God’s will is—his good, pleasing and perfect will.
Romans 12:2 (NIV)
Along with medication, Cognitive-Behavioral therapy (CBT) represents one of the two primary, evidence-based treatments for children and adolescents with Major Depression. Interpersonal Therapy (IPT) also has supporting evidence for effectiveness in pediatric depression, but far less than CBT.
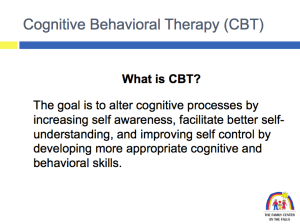 What exactly are we trying to do with kids through CBT? I’m including a slide (right) from a presentation Dr. Sherri McClurg from our practice uses to explain CBT in lectures with parents. Kids who experience depression and/or anxiety are especially vulnerable to “thinking errors.” The kids I treat are prone to what one of our therapists refers to as “stinking thinking”…automatic, irrational thoughts pop into their heads in the course of day-to- day living that trigger negative emotions and lead to patterns of self-defeating behavior. These patterns of self-defeating behaviors often reinforce their cognitive misperceptions and lead to a downward spiral resulting in symptoms of anxiety, depression, and sometimes, suicidal thoughts or plans. The job of the therapist is to help kids recognize the irrational thoughts and maladaptive patterns of behavior that contribute to negative emotions and help them to identify and implement alternative patterns of thinking and behavior in those situations when they’re most vulnerable to thinking errors. We’ll describe this to kids by telling them that we’re teaching them coping strategies or tools in order to give them the power to manage their emotions…helping them to develop a sense of competency.
What exactly are we trying to do with kids through CBT? I’m including a slide (right) from a presentation Dr. Sherri McClurg from our practice uses to explain CBT in lectures with parents. Kids who experience depression and/or anxiety are especially vulnerable to “thinking errors.” The kids I treat are prone to what one of our therapists refers to as “stinking thinking”…automatic, irrational thoughts pop into their heads in the course of day-to- day living that trigger negative emotions and lead to patterns of self-defeating behavior. These patterns of self-defeating behaviors often reinforce their cognitive misperceptions and lead to a downward spiral resulting in symptoms of anxiety, depression, and sometimes, suicidal thoughts or plans. The job of the therapist is to help kids recognize the irrational thoughts and maladaptive patterns of behavior that contribute to negative emotions and help them to identify and implement alternative patterns of thinking and behavior in those situations when they’re most vulnerable to thinking errors. We’ll describe this to kids by telling them that we’re teaching them coping strategies or tools in order to give them the power to manage their emotions…helping them to develop a sense of competency.
Here’s an excellent review article for parents summarizing the research and application of CBT in children and teens with depression from the journal Child and Adolescent Psychiatric Clinics of North America. One of the challenges in interpreting the data on CBT in kids involves the highly variable estimates of the effect size of the treatment (how much better do they get?) in kids with depression. This also points out the major functional limitation of a treatment plan for a child with depression that incorporates CBT- The child’s response is highly dependent upon the skill level and experience of the clinician providing the treatment.
We have a policy in our practice of not accepting referrals of kids who are involved in ongoing treatment with a clinician we don’t know. One reason I feel strongly about this is that I need to know what kids are getting if I’m being held responsible for their care. Not everybody who claims to be doing CBT with kids is actually providing a treatment that remotely resembles the therapy referenced in the article I linked to earlier in the post. While there’s a psychotherapeutic component to what I’m doing when I prescribe medication that (hopefully) contributes to the treatment effect, there’s less likely to be big difference in a kid’s response to Prozac based upon whether I’m the person writing the prescription as opposed to their pediatrician or nurse practitioner. After all, it’s all probably coming from the same jar at the CVS or Walgreen’s! The effectiveness of their CBT is highly dependent upon who’s doing the treatment. The lack of availability of well-trained clinicians in use of CBT with kids and teens creates enormous access problems for families.
Another functional limitation is the cost of CBT versus medication for kids with depression. In the two principal studies comparing CBT and medication in pediatric depression (the subject of our next post), kids received 12 sessions of CBT during the acute phase of treatment. A typical course of treatment for a kid with depression will involve around 20 visits with decreasing frequency over the course of a year. In our area, none of the three clinicians who I most frequently refer families to for CBT participate in insurance networks and their fee per session ranges from $125 to $140. One way of looking at the treatment is that it still costs less than my kid’s orthodontist and provides them with skills that last a lifetime. On the other hand, at $4/month, a year’s supply of Prozac will can cost a family under $50, and the copays for 4-6 follow up visits over the course of the year with their primary care physician or in-network psychiatrist may run from $100-$300. Given the state of the economy and the financial demands families are facing, cost all too often becomes the overriding consideration in treatment planning.
Finally, for many kids and families, the time required for effective CBT is a major impediment. Finding time to do CBT can be a big problem for teens when they’re “in-season” for their sport, or for kids in the performing arts when they’re preparing for a play or a recital. Between extracurricular activities and homework, it’s not uncommon for kids to tell me that the stress involved with blocking out time to come to therapy outweighs the benefits.
Bottom line…I encourage families to consider CBT before medication for their child or teen with depression when…
- Their child’s symptoms of depression are less severe.
- When their child’s mood state appears highly dependent upon their misperceptions and irrational patterns of thinking and behavior.
- A significant risk exists that antidepressant medication will exacerbate some other comorbid mental health condition or suicidal/self-injurious behavior. I’ll discuss this further in an upcoming post.
Photos courtesy of freedigitalphotos.net
***********************************************************************************************************
 Our Key Ministry team will be hitting the road to be part of the 2013 Accessibility Summit, hosted by McLean Bible Church in suburban Washington D.C. on April 19th-20th. This year’s Summit features Emily Colson (daughter of Chuck) As an artist, author, and speaker, Emily is passionate about inspiring others to persevere through their challenges and appreciate life’s gifts. In her book Dancing with Max, she and her late father share the struggle and beauty of life with Max, Emily’s son with autism.
Our Key Ministry team will be hitting the road to be part of the 2013 Accessibility Summit, hosted by McLean Bible Church in suburban Washington D.C. on April 19th-20th. This year’s Summit features Emily Colson (daughter of Chuck) As an artist, author, and speaker, Emily is passionate about inspiring others to persevere through their challenges and appreciate life’s gifts. In her book Dancing with Max, she and her late father share the struggle and beauty of life with Max, Emily’s son with autism.
For more on our Key Ministry presentations, click here. For more information on the Summit and registration, click on the Summit logo to the right.


Thanks for your clarity in walking readers through the specifics of how CBT differs from other therapies. In our family, we have found that it is not an either/or regarding meds or therapy, but a both/and. Neither tool would be as effective without the other. I wonder if most families find this to be true…
LikeLike
Pingback: Cognitive-Behavioral Therapy for kids with depression…pros and cons | ChristianBookBarn.com
Very nice summary Steve. Why more professionals wouldn’t want to use evidence-based approaches, I will never know. BTW, I think IPT is coming along as an EST…. It is probably just likely to work as CBT, but what I am hoping is that future work will help identify which approach might be best for which child. I have always thought that the fundamental difference between most child and adult clinical situations (not all, but most) is that initially, at least, the child doesn’t want to be there, or at least it was their idea. This puts them in a very different psychological space than the adult who is there saying, in effect, “Please help me.” I hope that psychologists will stop thinking about what theoretical “school” they are from and simply work on implementing the things we know that work… like CBT.
LikeLike
Pingback: Fix My Depression Now! – The Pineapple Newspaper | Depression Therapy:What Suits You Best
Pingback: Psychotherapy’s Image Problem – New York Times | Depression Therapy:What Suits You Best
Pingback: Emotion regulation training enhances efficacy of inpatient cognitive … – News-Medical.net | Depression Therapy:What Suits You Best
Pingback: The many shades of depression – U-T San Diego | Depression Therapy:What Suits You Best
Pingback: Choosing between Internet-based psychodynamic versus cognitive behavioral … – 7thSpace Interactive (press release) | Depression Therapy:What Suits You Best
Pingback: Cognitive behavioral therapy ‘effective’ for health anxiety – Medical News Today | Depression Therapy:What Suits You Best
Pingback: GINNY SUGIMOTO | Getting help for depression | Depression Therapy:What Suits You Best
Pingback: Largest therapy trial worldwide: Psychotherapy treats anorexia effectively | Depression Therapy:What Suits You Best
Pingback: Suicide: How You Can Make a Difference – PARADE | Depression Therapy:What Suits You Best
Pingback: Speak up to controlling husband – Waterloo Record | Depression Therapy:What Suits You Best
Pingback: A special bond – Hometownlife.com | Depression Therapy:What Suits You Best
Pingback: New Book Shows How to “Find the Path to Recovery,” and Get the Life You Want | Depression Therapy:What Suits You Best
Pingback: Ruby Wax: why mindfulness is the secret to a happy new year | Depression Therapy:What Suits You Best
Pingback: Sex is doctor's life's work | Depression Therapy:What Suits You Best
Pingback: Schools not required to screen for mental health problems | Depression Therapy:What Suits You Best
Pingback: Placerville Family Therapist, Kathleen Young MA, LMFT Provides Tips to … – Newswire (press release) | Depression Therapy:What Suits You Best
Pingback: Placenta popularity on the rise | Depression Therapy:What Suits You Best
Pingback: Girl testifies stepdad doctor 'waterboarded' her for vomiting milk | Depression Therapy:What Suits You Best
Pingback: Afraid of My Own Crazy – Huffington Post | Depression Therapy:What Suits You Best
Pingback: New Treatments For Depression » Blog Archive Therapy For Depression Cognitive
Pingback: New Treatments For Depression » Blog Archive Therapy For Depression Cbt
Pingback: New Treatments For Depression » Blog Archive Depression Therapy Pros And Cons